I have had several inquires regarding the use of kinesiology tape for the reduction of bruising and swelling. Questions have mostly related to the best method of application and exactly how something as simple as tape can reduce swelling of an extremity or bruising. In my view, sharing this information may be beneficial to clinicians and patients alike.Between 2007 and 2009, I completed a review of all literature available at that time regarding the use of kinesiology taping for clinical purposes, and the use of non-compressive taping techniques for assisting lymphatic function intrigued me. The available literature did not offer a logical description of exactly how non-compressive taping techniques can reduce the appearance of a bruise. After further reviewing literature, having discussions with anatomists and experimenting in the clinic, I believe I have been able to identify the actual mechanical role of kinesiology style taping in the enhancement of lymphatic function. This information is what I present in lecture as part of kinesiology taping instruction at the University of Utah’s schools of Physical Therapy, Athletic Training and Physical Medicine and Rehabilitation. For the sake of perspective, I would like to share an actual clinical case to illustrate one possible application of this technique.
Clinical Case Example:
I had a patient come into the clinic reporting that she tried a bit of archery at an acquaintance’s house in Colorado. She had apparently struck her left arm several times when releasing the arrows toward the intended target. Being a physical therapy doctoral student, she was aware of the benefit KT Tape has to offer in reducing bruising more quickly than leaving the bruise untreated. Here are a few snapshots we took with my phone while we taped her up.

Figure 1: Left arm prior to taping

Figure 2: Applying a proximal anchor with absolutely no stretch on the tape and arm positioned with skin on stretch. KT Tape is cut into strips to spread a single strip over a large area.

Figure 3: Arm positioned so skin is on stretch, no stretch on tape as it is applied

Figure 4: Applying remaining strips with no stretch on tape, continued stretch on skin through positioning

Figure 5: Taking care to place skin on stretch on opposite side of the elbow’s axis of rotation

Figure 6: All KT Tape from a single application in place

Figure 7: Notice the convolutions where the KT Tape lifts the skin. This is what creates a lymphatic assisting effect

Figure 8: Prior to KT Tape application

Figure 9: 24 hours after KT Tape application. Note the areas where the tape was applied and the marked reduction in ecchymosis/bruising
So the natural question after witnessing this effect of proper KT Tape application is;
“Very cool… but how’s that work?”
The Explanation:
The answer lies within the anatomy of our lymphatic system and the properties of KT Tape. The lymphatic system is part of and works with the circulatory system. While the circulatory system carries blood, the lymphatic system carries lymph, a cloudy fluid made up of blood plasma, lymphocytes, other white blood cells, proteins, cell waste products and other debris. While the circulatory system is a closed loop, the lymphatic system is an open-ended system and does not have a pump such as the heart. One of the lymphatic systems functions is to collect the fluid that is squeezed out of the circulatory system. As blood is pumped out of the heart it is under relatively high pressure, 120 mmHg to be exact, the first number, systolic pressure, when you have your blood pressure taken. This is so blood flow can continue through your body, and as blood flows into smaller and smaller divisions of the arterial tree it eventually reaches capillary beds. At the site of the capillary bed fluid is forced out of the capillaries into the extracellular space due to the pressure the blood is under. This fluid is not reabsorbed by the circulatory system and returned to the heart by the venous portion but rather it is absorbed by the open-ended lymphatic system.
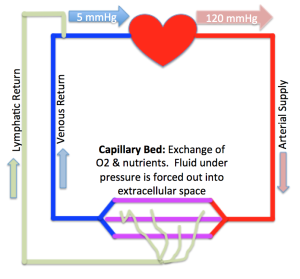
Figure 8: Basic diagram of lymphatic system
Though the entry of fluid and cells into lymphatics is not completely understood by anatomists at this time, it is known that lymphatic circulation begins with highly permeable, superficial lymph capillaries formed by endothelial cells with junctions between them that allows fluid to pass through with sufficient interstitial pressure. The junctions consist of protein filaments (Platelet Endothelial Call Adhesion Molecule-1 or PECAM-1) originally thought to have a protective or structurally supportive role, however is now believed to play a significant role in how extracellular fluid enters into the lymphatic system. These PECAM-1 filaments appear to be attached to the surrounding tissues and as the surrounding tissue moves, the filaments are pulled and released. This is thought to create a piston-like effect, opening and closing the lymphatic capillaries, also known as pre-lymphatics, allowing fluid to enter the system.
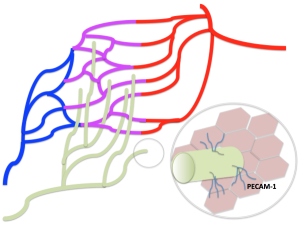
Figure 9: Location of PECAM-1 filaments, attached to surrounding tissues
To achieve a continuous lymphatic uptake of extracellular fluid, intermittent tissue stresses and movements need to occur. These surrounding tissue movements can be subtle and include:
- arterial pressure pulsations
- arteriolar vasomotion
- smooth muscle contractions and motilities
- skeletal muscle contraction
- skin tension
- external compression
What KT Tape enhances is the skin tension and release that occurs with natural active movement of the involved tissues. When applied with the proper technique, KT Tape exaggerates the motion of the subcutaneous PECAM-1 filaments, thus augmenting the body’s natural system of removing extracellular fluids and waste.

Figure 10: A closer look at the effect KT Tape has when applied using this method. Note the convolutions creating the lymphatic assist where the skin is in a position of “slack” vs. stretch
This exaggerated tissue movement can be seen in the convolutions of KT Tape strips in the images above, in this case, with elbow movement and the stretch and slackening of the skin over the area of the targeted bruise. The enhanced tissue movement then in turn amplifies the effect of PECAM-1 piston-like motion, offering an increase in extracellular fluid uptake by the pre-lymphatics. This is what decreases the observable bruising. Bruising is the breaking of capillaries and leakage of blood into the extracellular space. The venous portion of the circulatory system does not absorb the extracellular blood and debris, but rather these are collected by the lymphatic system. As blood cells and other debris are absorbed, the bruise turns lighter in color, from purples and reds to greens and yellows due to an effect of light waves refracting off the skin (your blood is not actually blue or green in color at any point in time despite what textbooks and my own illustrations depict). This technique also works very well for reduction of swelling over a joint, such as with ankle sprains or with post-surgical applications.
Applying KT Tape for Lymphatic Assist:
- Clean the area of application to remove any lotions or skin oils
- Cut KT Tape into strips, creating a “squid” or fork-like design
- Position the area where tape is to applied as to place the skin on stretch
- Place the anchor of the tape strip proximal and medial to the area of treatment
- Apply each cut portion of the KT Tape strip with absolutely no stretch over the area to be treated with the skin remaining on stretch
- Before moving the area out of a position of stretch, gently rub the KT Tape as to create friction for better adhesion
- Proper application will result in convolutions of the tape and skin once the area is returned to a normal position
For this technique to function optimally keep in mind:
Helpful Tips:
- Cut KT Tape into thin strips as to spread a single strip over a larger area
- Place the area to be taped so the skin is on much stretch as possible (within patient comfort and precautions)
- Anchor the KT Tape strip proximally and medially if possible as this follows the pattern of our neurovascular (and lymphatic) structures
- Apply KT Tape with absolutely no stretch on the tape itself over the target area
- Be aware of skin stretch if taping near joints, skin should be on relative stretch as tape is applied, this may require changing position of the joint as you tape
- If tape is applied properly, convolutions in the tape, pulling up gently on the skin should be observed
- Multiple strips can be used in conjunction with each other in a single application, creating lattice designs or “daisy-chaining” multiple strips along the entire extremity
- Movement must take place for KT Tape to enhance the extracellular fluid uptake, often needing nothing more than natural movement that takes place with activities of daily living
- Avoid taping over still healing incisions or wounds as not to avoid disturbing newly developing cells. You can however tape over post-surgical “steri-strips” with caution to avoid the incision itself
- Tape can be worn for 3-5 days, though remove if there are any complaints of itching or other discomfort of any kind
Other Kinesiology Taping for Lymphatic Assist Precautions:
- Consult your physician or therapist before taping with this technique if you have as part of your past medical history
- Cancer
- Active Infection
- Radiation Burns
- Congestive Heart Failure
- Renal Insufficiency
- DVT (Deep Vein Thrombosis)
- Remove tape if you experience:
- Deep ache with tape
- “Tingle” or Numbness
- Skin is “itchy” under or near tape
- Tape “just doesn’t feel good”
I hope this helps to de-mystify the lymphatic technique and effects of KT Tape in lymphatic enhancement!
Please contact our clinic if you have any comments or concerns and happy taping!
Christopher Harper, PT, DPT, OCS Doctor of Physical Therapy/Board Certified Orthopedic Specialist
Active Lifestyles Physical Therapy
11760 South 700 East, Suite 211
Draper, Utah 84020
PH: (801) 456-9900 FX: (801) 456-9899
References:
1. Baluk P, et al. Functionally specialized junctions between endothelial cells of lymphatic vessels. J Exp Med. 2007 Oct 1; 204 (10):2349-62
2. Daroczy J. New structural details of dermal lymphatics valves and its functional interpretation. Lymphology. 1984 Jun; 17 (2); 54-60
3. Schmid-Schönbein GW. Microlymphatics and Lymph Flow. Physiol Rev. 1990 Oct; 70 (4); 987-1028
Author: Christopher Harper, PT, DPT, OCS
